When a doctor taps on your chest with a stethoscope and you hear a dull, muffled sound instead of a clear, crisp one, it could be an indication of something amiss with your lungs. Dullness to percussion, as it is known in medical terminology, is a common finding in patients with respiratory illnesses, and can signal a range of conditions from mild to severe. In this article, we will explore what dullness to percussion means in the context of lung health, and what it could signify about your respiratory system. So, buckle up and prepare to take a deep dive into the world of lung diagnosis!
Dullness to percussion in the lungs can indicate the presence of fluid, pus, or mucus in the lungs. This can be a sign of various conditions such as pneumonia, bronchitis, or lung abscess. It is important to note that dullness to percussion is not a diagnostic tool, but rather a finding that may suggest further evaluation and testing. If you are experiencing symptoms such as difficulty breathing, chest pain, or cough, it is important to see a healthcare provider for proper diagnosis and treatment.
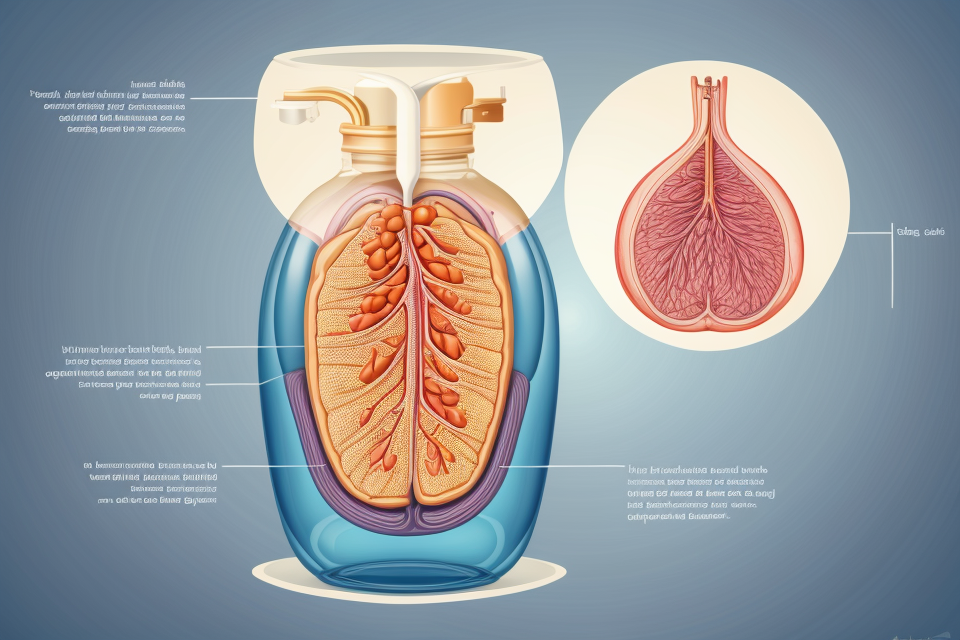
What is percussion in the lungs?
How is percussion performed?
Percussion is a technique used by healthcare professionals to assess the condition of the lungs and other internal organs. It involves tapping on the chest or back with a small, blunt instrument called a percussion hammer. The sound that is produced when the hammer strikes the chest or back provides important information about the condition of the lungs and other organs.
Dullness to percussion is a term used to describe a specific type of sound that is heard when the percussion hammer is tapped on the chest or back. This sound is different from the normal percussion sound and is often described as being “dull” or “muffled.” Dullness to percussion can indicate a number of different conditions, including:
- Fluid accumulation in the lungs (pleural effusion)
- Consolidation or thickening of the lung tissue (pneumonia, interstitial lung disease)
- Reduced air spaces in the lungs (atherosclerosis, pulmonary fibrosis)
- Compression of the lungs by a tumor or other mass
In order to diagnose the underlying cause of dullness to percussion, healthcare professionals may use a variety of additional tests and diagnostic tools, including chest x-rays, CT scans, and blood tests. Treatment will depend on the underlying cause of the dullness to percussion and may include medications, oxygen therapy, or other interventions.
What are the normal findings on percussion?
During a physical examination, a healthcare provider may use percussion to assess the condition of the lungs. Percussion involves tapping on the chest or back with a small, blunt instrument, such as a reflex hammer, to produce a characteristic sound that can indicate the presence or absence of various lung conditions.
When the chest or back is struck with the instrument, the sound that is produced is known as a “chest note.” This note is usually described as either “clear” or “dull,” depending on the characteristics of the sound. In the context of lung examination, a clear chest note is generally considered to be a normal finding, while a dull chest note may indicate the presence of fluid, pus, or other abnormal substances in the lungs.
The normal findings on percussion can vary depending on the individual’s age, overall health, and other factors. In general, a clear chest note is typically heard over most of the lung fields, with the exception of the lungs’ lower lobes, where the sound may be dull due to the presence of the diaphragm. In addition, the sound may be slightly louder over the lungs’ upper lobes, where the air is more resonant.
In summary, a clear chest note is generally considered to be a normal finding on percussion, while a dull chest note may indicate the presence of fluid, pus, or other abnormal substances in the lungs. The specific characteristics of the chest note can provide important clues about the patient’s respiratory health and may help guide further diagnosis and treatment.
What are the abnormal findings on percussion?
Percussion is a diagnostic technique used by healthcare professionals to assess the condition of the lungs. During the examination, a clinician uses a small, tapered hammer to tap on the chest wall, and then listens for any sounds produced by the lungs. These sounds can provide valuable information about the condition of the lungs, such as whether they are filled with air or fluid, or whether there are any obstructions in the airways.
There are several normal findings on percussion, including:
- Voided sounds: These are high-pitched sounds that are heard when the lungs are empty.
- Respiratory sounds: These are low-pitched sounds that are heard when the lungs are filled with air.
- Tactile fremitus: This is a vibration felt by the clinician’s hand when the lungs are filled with air.
However, there are also several abnormal findings on percussion that can indicate various lung conditions. These include:
- Ronchi’s sign: This is a flat, dull sound that is heard when the lungs are filled with fluid or mucus.
- Vesicular breath sounds: These are high-pitched, moist sounds that are heard when the lungs are filled with air, but the air is trapped in small pockets in the lungs. This can indicate pulmonary congestion or edema.
- Decreased or absent breath sounds: This can indicate that the lungs are not functioning properly, or that there is an obstruction in the airways.
- Lung crackles: These are sharp, high-pitched sounds that are heard when the lungs are filled with air, but there are obstructions in the airways. This can indicate pneumonia or bronchitis.
- Bronchial breathing: This is a low-pitched, humming sound that is heard when the air is moving through narrowed or obstructed airways. This can indicate asthma or chronic obstructive pulmonary disease (COPD).
It is important to note that while these abnormal findings on percussion can indicate various lung conditions, they are not diagnostic in and of themselves. Further testing and evaluation may be necessary to determine the underlying cause of these findings.
What is dullness to percussion?
What causes dullness to percussion?
Dullness to percussion is a medical term used to describe a reduced or absent sound when a healthcare professional taps on a patient’s chest with a stethoscope. This phenomenon can occur in various parts of the body, but it is most commonly associated with the lungs.
There are several potential causes of dullness to percussion in the lungs, including:
- Consolidation: When the air spaces in the lungs become filled with fluid, pus, or solid material, such as blood, the sound of percussion is dulled or muffled. This is because the material present in the lungs is not capable of vibrating and producing a clear sound.
- Air trapping: In cases of certain lung diseases, such as asthma or chronic obstructive pulmonary disease (COPD), the airways may become inflamed and narrowed, causing a build-up of air in the lungs. This can lead to dullness to percussion, as the sound waves are unable to travel through the air-filled spaces in the lungs.
- Pleural effusion: A buildup of fluid in the space between the lungs and the chest wall can also cause dullness to percussion. This fluid acts as a barrier to the sound waves, reducing their ability to transmit clearly.
- Pneumothorax: A pneumothorax is a condition in which air leaks from the lungs into the space between the lungs and the chest wall. This can result in dullness to percussion, as the sound waves are absorbed by the air in this space.
- Lung collapse: In some cases, a portion of the lung may collapse, reducing the amount of air present and leading to dullness to percussion. This can occur due to various factors, such as trauma or underlying lung disease.
It is important to note that dullness to percussion is not always indicative of a specific medical condition. In some cases, it may simply be a sign of poor lung function or other factors. However, it is a common finding in patients with lung disease and can be used as an important diagnostic tool by healthcare professionals.
How is dullness to percussion characterized?
Dullness to percussion is a physical examination finding that occurs when a healthcare provider taps on a patient’s chest with a stethoscope and the sound that is heard is dull or muffled. This finding is typically associated with lung conditions that cause inflammation or fluid buildup in the lungs, such as pneumonia or pulmonary edema.
Dullness to percussion can be characterized by several features, including:
- Decreased resonance: When a patient has dullness to percussion, the sound that is heard through the stethoscope is typically weaker and less resonant than normal. This is because the inflammation or fluid buildup in the lungs dampens the sound.
- Increased difficulty hearing: Healthcare providers may have difficulty hearing the sound of dullness to percussion because it is muffled or obscured by other sounds. This can make it more challenging to diagnose certain lung conditions.
- Presence of other findings: Dullness to percussion is often accompanied by other physical examination findings, such as decreased breath sounds or increased respiratory rate. These findings can help healthcare providers determine the underlying cause of the dullness to percussion.
Overall, dullness to percussion is an important physical examination finding that can indicate a range of lung conditions. Healthcare providers use this finding, along with other clinical findings and diagnostic tests, to diagnose and treat lung conditions in their patients.
How is dullness to percussion differentiated from other findings on percussion?
Dullness to percussion is a medical finding that refers to a decreased or muffled sound that is heard when a healthcare provider taps on a patient’s chest with a stethoscope. This finding is typically indicative of a problem with the lungs or the surrounding tissues.
In order to differentiate dullness to percussion from other findings on percussion, healthcare providers will consider a number of factors. These may include:
- The location of the dullness: Dullness to percussion may be heard in different parts of the chest, depending on the underlying cause. For example, dullness may be heard over the lungs if there is fluid or inflammation in the lungs, while dullness may be heard over the heart if there is fluid in the pericardial sac.
- The quality of the dullness: The quality of the dullness may provide additional clues as to the underlying cause. For example, dullness that is heard over the lungs may be described as “muffled” or “decreased,” while dullness that is heard over the heart may be described as “loud” or “systolic.”
- The presence of other findings: In addition to dullness to percussion, healthcare providers may also listen for other findings on percussion, such as decreased or increased vocal fremitus (vibration of the chest wall). These findings may provide additional clues as to the underlying cause of the dullness.
Overall, the ability to differentiate dullness to percussion from other findings on percussion is an important skill for healthcare providers, as it can help them to accurately diagnose and treat a wide range of medical conditions.
How is dullness to percussion diagnosed?
When a physician performs a physical examination, one of the diagnostic tools used is percussion. Percussion is the act of tapping on the chest or back with a small, padded instrument called a hammer. The sound that is produced by the tapping can provide valuable information about the condition of the lungs. Dullness to percussion refers to a lack of resonance or a muffled sound when the physician taps on the chest or back.
Dullness to percussion can be an indication of several different conditions, including fluid accumulation in the lungs, pneumonia, or lung cancer. Therefore, it is important for physicians to carefully assess the sound produced during percussion and consider other diagnostic tests to determine the underlying cause of the dullness.
In order to diagnose the cause of dullness to percussion, physicians may use a variety of diagnostic tools, including:
- Chest X-ray: This imaging test can provide detailed images of the lungs and can help identify any abnormalities, such as fluid accumulation or tumors.
- Blood tests: Blood tests can be used to assess the overall health of the body and to check for signs of infection or inflammation.
- Lung function tests: These tests measure how well the lungs are functioning and can help identify any abnormalities or restrictions in lung function.
- CT scan: A CT scan is a detailed imaging test that can provide cross-sectional images of the body. It can be used to assess the lungs and other organs for signs of disease.
In addition to these tests, physicians may also consider the patient’s medical history, symptoms, and physical examination findings to determine the underlying cause of dullness to percussion. It is important for patients to follow their physician’s recommendations and undergo any necessary diagnostic tests in order to accurately diagnose and treat any underlying conditions.
What are the potential complications of dullness to percussion?
Dullness to percussion is a medical term used to describe a decreased or absent sound heard when a healthcare provider taps on a particular area of the body with a stethoscope. In the context of the lungs, dullness to percussion may indicate the presence of fluid, pus, or other substances in the lungs, which can impede the transmission of sound.
The potential complications of dullness to percussion in the lungs may include:
- Pneumonia: Infection of the lungs that can cause inflammation and accumulation of fluid or pus in the lungs, leading to dullness to percussion.
- Atelectasis: Collapse or deflation of a part of the lung, which can result in decreased or absent breath sounds and dullness to percussion.
- Pleural effusion: Accumulation of fluid in the space between the lungs and the chest wall, which can result in dullness to percussion.
- Consolidation: The presence of fluid or pus in the air spaces of the lungs, which can result in decreased or absent breath sounds and dullness to percussion.
- Lung cancer: Tumors in the lungs can cause dullness to percussion if they obstruct airflow or impede the transmission of sound.
It is important to note that dullness to percussion is not always indicative of a serious condition, and may be a normal finding in certain circumstances, such as during pregnancy or in individuals with certain medical conditions. However, in certain cases, dullness to percussion may be a sign of a more serious underlying condition that requires prompt medical attention. Therefore, it is important to consult a healthcare provider for proper evaluation and management.
How is dullness to percussion treated?
What are the goals of treatment for dullness to percussion?
The primary goal of treatment for dullness to percussion in the lungs is to alleviate the underlying cause of the symptom. This may involve addressing any underlying respiratory infections or conditions that may be contributing to the dullness, such as chronic obstructive pulmonary disease (COPD) or asthma. In some cases, treating the underlying condition may resolve the dullness to percussion entirely.
Another goal of treatment is to manage any accompanying symptoms or complications associated with dullness to percussion. This may include providing relief from cough, shortness of breath, or chest pain, and addressing any potential issues with oxygenation or ventilation.
In addition, treatment for dullness to percussion may also involve managing any contributing factors such as smoking or exposure to air pollution, and addressing any underlying cardiovascular or pulmonary issues that may be contributing to the symptom.
Overall, the goals of treatment for dullness to percussion are to address the underlying cause of the symptom, manage any accompanying symptoms or complications, and promote overall respiratory health and function.
What are the options for treating dullness to percussion?
There are several options for treating dullness to percussion in the lungs, depending on the underlying cause of the symptom. One option is to use antibiotics to treat any underlying bacterial infections that may be present. This is particularly important if the dullness to percussion is accompanied by other symptoms such as cough, fever, or difficulty breathing.
Another option is to use bronchodilators to open up the airways and improve breathing. This may be particularly effective in cases where the dullness to percussion is caused by inflammation or constriction of the airways.
In some cases, treatment may involve using a nebulizer to deliver medication directly to the lungs. This can be particularly effective in cases where the lungs are inflamed or congested, as it allows the medication to be delivered directly to the affected area.
In addition to medication, there are several lifestyle changes that can help to improve lung function and reduce dullness to percussion. These may include quitting smoking, avoiding exposure to pollutants and irritants, and engaging in regular exercise to improve lung capacity.
It is important to note that the best course of treatment for dullness to percussion will depend on the underlying cause of the symptom. A healthcare professional should be consulted to determine the most appropriate treatment plan for each individual case.
What is the prognosis for patients with dullness to percussion?
Prognosis for patients with dullness to percussion can vary depending on the underlying cause of the condition. Generally, if the dullness to percussion is caused by a respiratory infection, the prognosis is good and the patient can expect to make a full recovery with appropriate treatment. However, if the dullness to percussion is caused by a more serious underlying condition such as lung cancer, the prognosis may be poor and the patient may require more extensive treatment or may not be able to be cured. In some cases, dullness to percussion may be a sign of a chronic condition that requires ongoing management and treatment to prevent further complications.
What is the role of follow-up care for patients with dullness to percussion?
The Importance of Follow-up Care for Patients with Dullness to Percussion
Patients who experience dullness to percussion in the lungs require careful follow-up care to ensure that their condition is properly managed and that any potential complications are promptly addressed. Follow-up care typically involves regular check-ups with a healthcare provider, who will monitor the patient’s condition and adjust their treatment plan as needed.
Some of the key elements of follow-up care for patients with dullness to percussion include:
- Monitoring for changes in symptoms: Patients with dullness to percussion may experience a range of symptoms, including cough, shortness of breath, and chest pain. It is important for healthcare providers to monitor these symptoms closely, as changes in symptoms can indicate the need for adjustments to the patient’s treatment plan.
- Tracking the patient’s vital signs: Healthcare providers will also monitor the patient’s vital signs, such as their heart rate, blood pressure, and oxygen levels, to ensure that their condition is stable and that their treatment is effective.
- Imaging studies: Imaging studies, such as chest X-rays or CT scans, may be used to assess the patient’s lung function and to detect any potential complications, such as pneumonia or atelectasis.
- Pulmonary function tests: Pulmonary function tests may be used to assess the patient’s lung function and to detect any potential abnormalities, such as reduced lung capacity or obstruction.
- Medication management: Patients with dullness to percussion may require medication to manage their symptoms and to treat any underlying conditions. Healthcare providers will monitor the patient’s response to medication and adjust their treatment plan as needed.
By providing ongoing follow-up care, healthcare providers can help patients with dullness to percussion manage their condition effectively and reduce the risk of complications. This may involve adjusting the patient’s treatment plan, providing education and support, and coordinating care with other healthcare providers as needed. With appropriate follow-up care, patients with dullness to percussion can improve their lung function and achieve a better quality of life.
FAQs
1. What is dullness to percussion in the lungs?
Dullness to percussion in the lungs refers to a decreased or muffled sound that is heard when a healthcare provider taps on the chest or back with a stethoscope. This is usually caused by fluid, pus, or air building up in the lungs, which can cause a reduction in the vibrations that are transmitted to the stethoscope.
2. What causes dullness to percussion in the lungs?
Dullness to percussion in the lungs can be caused by a variety of conditions, including pneumonia, pleurisy, lung abscess, and pulmonary edema. These conditions can all lead to the accumulation of fluid, pus, or air in the lungs, which can result in a decrease in the sound that is transmitted to the stethoscope.
3. How is dullness to percussion diagnosed?
Dullness to percussion is typically diagnosed by a healthcare provider using a stethoscope. The provider will listen for abnormal sounds in the lungs, such as decreased or muffled sounds, and will also examine the patient for other signs and symptoms of lung disease. In some cases, additional tests such as X-rays or CT scans may be ordered to help confirm the diagnosis.
4. What is the treatment for dullness to percussion in the lungs?
The treatment for dullness to percussion in the lungs will depend on the underlying cause of the condition. In some cases, the fluid or air accumulation may resolve on its own without any treatment. In other cases, treatment may involve medications to clear the fluid or air, or procedures such as thoracentesis or chest tube insertion to remove the fluid or air. In severe cases, hospitalization may be necessary.
5. Is dullness to percussion a serious condition?
Dullness to percussion in the lungs can be a sign of a serious underlying condition, such as pneumonia or lung abscess. However, the severity of the condition will depend on the underlying cause and the overall health of the patient. In some cases, dullness to percussion may be a mild and temporary condition that resolves on its own with rest and hydration. In other cases, it may be a sign of a more serious and potentially life-threatening condition that requires immediate medical attention.