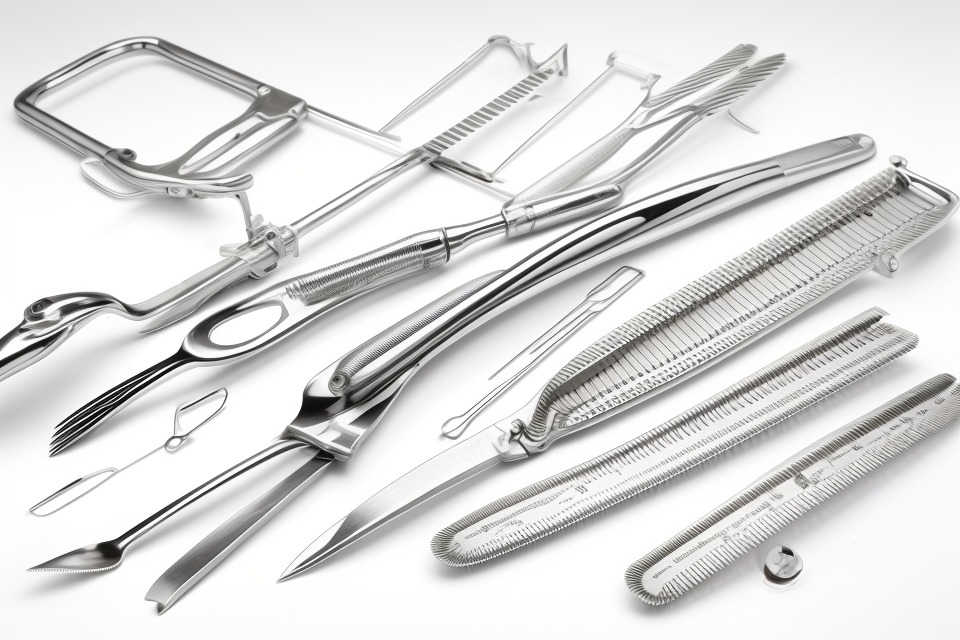
Surgical instruments are an essential part of any medical facility, and their proper care and maintenance is crucial to ensuring the safety and well-being of patients. However, with the numerous types of surgical instruments available, knowing how to care for them can be a daunting task. This guide provides a comprehensive overview of the best practices for cleaning, maintaining, and storing surgical instruments, to help healthcare professionals keep their instruments in optimal condition. Whether you’re a seasoned professional or just starting out, this guide has something for everyone. So, let’s dive in and explore the world of surgical instrument care!
Understanding the Importance of Surgical Instrument Care
Why is proper care essential for surgical instruments?
Proper care is essential for surgical instruments as they are used in critical medical procedures, and even the slightest contamination or damage can lead to severe consequences. In addition, surgical instruments are expensive, and proper care can help extend their lifespan and reduce the need for frequent replacements.
Furthermore, surgical instruments are made of various materials, including metal, plastic, and ceramic, which can corrode or degrade over time if not properly maintained. Proper care also helps maintain the sharpness and accuracy of the instruments, ensuring optimal performance during surgical procedures.
In summary, proper care is crucial for surgical instruments as it ensures patient safety, extends the lifespan of the instruments, and maintains their performance.
The impact of improper care on patient safety and instrument longevity
Improper care of surgical instruments can have a significant impact on patient safety and instrument longevity. Inadequate cleaning and sterilization can lead to the spread of infection, while poor maintenance can result in damage to the instruments and reduce their effectiveness. This section will explore the ways in which improper care can negatively affect patient safety and instrument longevity.
- Infection control:
- Inadequate cleaning and sterilization can lead to the spread of infection from one patient to another, which can have serious consequences for patient health.
- Improper care can also lead to the buildup of biofilm, which can be difficult to remove and can harbor harmful bacteria.
- Instrument damage:
- Poor maintenance can result in damage to the instruments, such as dents, cracks, or corrosion.
- This damage can reduce the effectiveness of the instruments and can even make them unsafe to use.
- Instrument longevity:
- Proper care can help to extend the lifespan of surgical instruments, reducing the need for frequent replacements and saving healthcare facilities money.
- Failure to maintain instruments properly can result in premature wear and tear, which can reduce their effectiveness and shorten their lifespan.
Overall, proper care of surgical instruments is essential for ensuring patient safety and instrument longevity. The following sections will provide guidance on best practices for cleaning, maintenance, and storage of surgical instruments.
Key benefits of following best practices for instrument care
Implementing best practices for surgical instrument care has numerous advantages for healthcare professionals and patients alike. By ensuring that instruments are properly cleaned, maintained, and stored, the risk of infection, injury, and equipment failure is significantly reduced. Some of the key benefits of following these best practices are as follows:
- Proper sterilization: The primary goal of surgical instrument care is to ensure that all instruments are properly sterilized before use. By following best practices, healthcare professionals can reduce the risk of infection for patients, which is especially important for those with compromised immune systems.
- Extended equipment lifespan: Regular maintenance and cleaning can help extend the lifespan of surgical instruments. By keeping instruments clean and well-maintained, healthcare professionals can avoid costly repairs or replacements that can disrupt patient care.
- Efficient workflow: Following best practices for instrument care can also improve workflow in the operating room. By ensuring that instruments are properly organized and easily accessible, healthcare professionals can reduce the time spent searching for or setting up equipment, allowing them to focus on providing high-quality patient care.
- Increased patient safety: Proper instrument care also plays a crucial role in patient safety. By ensuring that instruments are free from contamination and functioning correctly, healthcare professionals can reduce the risk of injury or complications during surgery.
- Compliance with regulations: Following best practices for instrument care is also essential for compliance with regulatory requirements. Healthcare facilities must adhere to strict guidelines set forth by accreditation bodies, such as the Joint Commission, to maintain their accreditation status. By implementing best practices for instrument care, healthcare professionals can ensure that their facility remains in compliance with these guidelines.
Types of Surgical Instruments and Their Unique Care Requirements
Handheld instruments
Handheld instruments are the most commonly used surgical instruments and require special care to maintain their quality and functionality. Here are some best practices for cleaning, maintenance, and storage of handheld instruments:
- Cleaning: Handheld instruments should be cleaned thoroughly after each use to prevent the buildup of biofilm and the spread of infection. Use a mild detergent and warm water to clean the instruments, making sure to remove any residual blood or tissue. It is important to inspect the instruments for any damaged or worn parts that may need to be replaced.
- Maintenance: Regular maintenance is essential to ensure the proper functioning of handheld instruments. This includes oiling moving parts, sharpening blades, and inspecting the instruments for any signs of wear or damage. Maintenance should be performed by trained professionals who understand the specific care requirements of each instrument.
- Storage: Handheld instruments should be stored in a clean, dry, and well-ventilated area. It is important to keep the instruments organized and labeled to prevent confusion and damage during transport. Covers or protective cases should be used to protect the instruments from dust and other debris. Additionally, instruments that require sterilization should be stored in a sterile or clean environment to prevent contamination.
In summary, handheld instruments require special care to maintain their quality and functionality. Cleaning, maintenance, and storage are critical steps in ensuring the proper functioning of these instruments and preventing the spread of infection.
Electrosurgical devices
Electrosurgical devices, such as electrosurgical pencils and electrodes, are designed to cut or coagulate tissue during surgical procedures. These devices use high-frequency electrical currents to heat and vaporize tissue, making them highly effective in various surgical applications. However, they also require specific care and maintenance to ensure their optimal performance and longevity.
- Cleaning: Electrosurgical devices should be cleaned immediately after use to prevent the buildup of organic matter, which can lead to malfunction and cross-contamination. Manufacturers usually provide specific cleaning instructions for their devices, which should be followed carefully. It is essential to use a high-quality detergent designed for use with electrosurgical instruments and to avoid using abrasive materials, as these can damage the device’s surfaces.
- Maintenance: Electrosurgical devices often require regular maintenance to ensure optimal performance. This may include inspecting the device for damage, cleaning or replacing parts, and checking for proper function. Some devices may also require calibration to ensure the electrical current is within safe and effective parameters. Manufacturers usually provide guidelines for regular maintenance, which should be followed to prevent malfunction and extend the device’s lifespan.
- Storage: Electrosurgical devices should be stored in a clean, dry environment away from direct sunlight and moisture. They should be kept separate from other instruments to prevent damage and cross-contamination. It is also essential to store the devices according to the manufacturer’s instructions, as some devices may require specific storage conditions to maintain their performance and longevity.
By following these best practices for cleaning, maintenance, and storage, healthcare professionals can ensure that electrosurgical devices remain safe and effective tools for surgical procedures.
Powered instruments
Powered surgical instruments, such as drills, saws, and burrs, require special care and maintenance due to their high speed and mechanical components. These instruments must be properly cleaned and sterilized after each use to prevent the spread of infection.
Here are some best practices for cleaning and maintaining powered surgical instruments:
- Remove all debris and residue from the instrument after each use.
- Use a disinfectant solution to thoroughly clean the instrument, paying particular attention to any crevices or joints where bacteria may accumulate.
- Dry the instrument thoroughly with a clean cloth or paper towel to prevent rust or corrosion.
- Lubricate moving parts as needed to prevent friction and wear.
- Store the instrument in a dry, clean, and well-ventilated area to prevent damage from moisture or corrosion.
In addition to these general care practices, some powered instruments may require additional maintenance or repair. For example, saws and drills may need their blades sharpened or replaced periodically, while burrs may need to be resharpened or replaced entirely.
It is important to follow the manufacturer’s instructions for cleaning and maintaining powered surgical instruments, as these instruments can be expensive and may require specialized care to function properly. Proper care and maintenance of powered instruments can help to ensure that they continue to function smoothly and safely during surgical procedures.
Other specialized instruments
Surgical instruments come in a variety of shapes, sizes, and functions, each with their unique care requirements. Among these specialized instruments are those that are not commonly used in everyday procedures but are crucial in specific medical specialties. Here are some examples of other specialized instruments and their unique care requirements:
Neurosurgical instruments
Neurosurgical instruments are designed for use in neurosurgeries, such as operations on the brain and spine. These instruments are usually delicate and have fine tips to prevent damage to sensitive tissues. They also often have a locking mechanism to ensure precise movements during surgery. Some examples of neurosurgical instruments include:
- Micro-instruments: These are small instruments used for precise movements during neurosurgeries. They are usually made of stainless steel or titanium and require careful cleaning and storage to prevent damage.
- Ultrasonic instruments: These instruments use high-frequency vibrations to cut through tissue during neurosurgeries. They require special care to prevent damage to the delicate tips and blades.
Ophthalmic instruments
Ophthalmic instruments are designed for use in eye surgeries, such as cataract removal and LASIK. These instruments are often small and delicate, with sharp edges that can cause damage if not handled properly. Some examples of ophthalmic instruments include:
- Phacoemulsification instruments: These instruments are used to break up the lens during cataract surgery. They require careful cleaning and sterilization to prevent the spread of infection.
- Microkeratome blades: These blades are used to make a flap in the cornea during LASIK surgery. They require careful handling and storage to prevent damage to the blade.
Cardiovascular instruments
Cardiovascular instruments are designed for use in heart surgeries, such as open-heart surgery and angioplasty. These instruments are often large and heavy-duty, with sharp edges and points that can cause damage if not handled properly. Some examples of cardiovascular instruments include:
- Aortic clamps: These instruments are used to clamp the aorta during heart surgery. They require careful cleaning and sterilization to prevent the spread of infection.
- Coronary artery bypass grafting instruments: These instruments are used to perform coronary artery bypass grafting surgery. They require careful handling and storage to prevent damage to the instruments.
Proper care and maintenance of these specialized instruments are crucial to ensure their effectiveness and longevity. Failure to follow best practices for cleaning, maintenance, and storage can result in damage to the instruments, decreased effectiveness, and even patient safety concerns. Therefore, it is essential to follow the best practices outlined in this guide for all types of surgical instruments, including these specialized instruments.
Cleaning and Preparation Techniques for Surgical Instruments
The importance of aseptic technique in instrument care
Maintaining aseptic technique is crucial for ensuring the sterility of surgical instruments. This technique involves the use of strict protocols to prevent the introduction of any contaminants into the sterile field during the cleaning, preparation, and storage of surgical instruments. The goal of aseptic technique is to minimize the risk of surgical site infections and other complications that can arise from the use of contaminated instruments.
One of the key principles of aseptic technique is to use sterile instruments and equipment whenever possible. This means that all instruments and equipment that come into contact with the sterile field should be sterilized using a validated sterilization process before use. Additionally, all instruments and equipment should be wrapped or covered to maintain their sterility until they are ready to be used.
Another important aspect of aseptic technique is the use of strict hand hygiene protocols. This includes washing hands with soap and water or using an alcohol-based hand sanitizer before and after handling instruments and equipment. Gloves should also be worn at all times when handling instruments and equipment to prevent the transfer of bacteria and other contaminants.
Finally, it is important to maintain a clean and organized environment in which to work. This includes cleaning and disinfecting all surfaces and equipment regularly, as well as storing instruments and equipment in designated areas to prevent contamination and cross-contamination. By following these guidelines, healthcare professionals can help ensure the safety and efficacy of surgical procedures and minimize the risk of complications.
Step-by-step guide to cleaning surgical instruments
- Preparation:
- Remove any disposable components
- Check for any damage or wear
- Record the instrument’s condition
- Disinfection:
- Immerse the instrument in a disinfectant solution
- Use an enzymatic cleaner for protein-based soils
- Soak for the recommended time
- Cleaning:
- Scrub the instrument with a non-abrasive brush
- Use a detergent solution for general cleaning
- Pay extra attention to hinges, locks, and other moving parts
- Rinse:
- Rinse the instrument thoroughly with water
- Use a sterile saline solution for delicate instruments
- Dry the instrument with a clean cloth or paper towel
- Inspect:
- Check for any remaining debris or residue
- Ensure all components are present and undamaged
- Document the instrument’s condition for maintenance purposes
- Packaging and storage:
- Use a clean, dry container
- Store instruments in a designated area or cabinet
- Consider using individual sleeves or wraps for each instrument
- Quality control:
- Implement regular maintenance and inspection schedules
- Train staff on proper cleaning and maintenance techniques
- Conduct regular audits to ensure compliance with best practices
By following this step-by-step guide, healthcare professionals can ensure that surgical instruments are thoroughly cleaned, disinfected, and maintained for optimal performance and safety.
Decontamination and sterilization processes
Decontamination and sterilization processes are critical steps in ensuring the safety and efficacy of surgical instruments. These processes aim to eliminate or inactivate all forms of microorganisms, including bacteria, viruses, and fungi, that may pose a risk to patients and healthcare personnel.
The following are the key steps involved in decontamination and sterilization processes:
Step 1: Preparation of instruments
The first step in decontamination and sterilization processes is the preparation of surgical instruments. This involves the removal of any debris, blood, or other contaminants that may be present on the instruments. This can be achieved through a process known as mechanical cleaning, which involves the use of brushes, scouring pads, or other abrasive materials to remove visible debris.
Step 2: Chemical cleaning
Once the instruments have been mechanically cleaned, they are then subjected to chemical cleaning. This involves the use of detergents, disinfectants, or other chemical agents to remove any residual contaminants that may not have been removed through mechanical cleaning. Chemical cleaning can be performed using various methods, including immersion, wiping, or spraying.
Step 3: Sterilization
After chemical cleaning, the instruments are then subjected to sterilization. Sterilization is the process of killing or inactivating all forms of microorganisms on the instruments. There are several methods of sterilization, including:
- Steam sterilization: This involves exposing the instruments to steam under pressure, which kills microorganisms by destroying their cell walls.
- Chemical sterilization: This involves the use of chemical agents, such as ethylene oxide or formaldehyde, to kill microorganisms.
- Radiation sterilization: This involves the use of ionizing radiation, such as gamma rays or X-rays, to kill microorganisms.
Step 4: Packaging and storage
After sterilization, the instruments are then packaged and stored in a sterile environment to prevent recontamination. This can be achieved through the use of sterile wrap, containers, or other sterile packaging materials. The instruments should be stored in a clean, dry, and well-ventilated area, away from sources of heat, moisture, or contamination.
Overall, proper decontamination and sterilization processes are critical to ensuring the safety and efficacy of surgical instruments. These processes should be performed regularly and in accordance with established guidelines and protocols to minimize the risk of infection and contamination.
Maintenance and Servicing of Surgical Instruments
Regular maintenance tasks for different types of instruments
To ensure the optimal performance and longevity of surgical instruments, regular maintenance is essential. Different types of instruments require specific care and attention. This section will provide an overview of regular maintenance tasks for various types of surgical instruments.
Scissors and Metzenbaum Scissors
- Clean instruments thoroughly after each use, removing any tissue residue or debris.
- Lubricate the blades periodically to reduce friction and maintain a sharp cutting edge.
- Inspect the scissors for any damage or wear, and replace them if necessary.
Hemostats
- Clean hemostats after each use, using a mild detergent solution or an enzymatic cleaner.
- Inspect the tips for any damage or wear, and replace them if necessary.
- Store hemostats in a clean, dry environment to prevent corrosion.
Forceps
- Clean forceps after each use, using a mild detergent solution or an enzymatic cleaner.
- Inspect the tips and joints for any damage or wear, and replace them if necessary.
- Store forceps in a clean, dry environment to prevent corrosion.
Tweezers
- Clean tweezers after each use, using a mild detergent solution or an enzymatic cleaner.
- Store tweezers in a clean, dry environment to prevent corrosion.
Rongeurs
- Clean rongeurs after each use, using a mild detergent solution or an enzymatic cleaner.
- Inspect the tips and blades for any damage or wear, and replace them if necessary.
- Store rongeurs in a clean, dry environment to prevent corrosion.
Scalpels
- Clean scalpels after each use, using a mild detergent solution or an enzymatic cleaner.
- Lubricate the blade periodically to reduce friction and maintain a sharp cutting edge.
- Inspect the scalpel for any damage or wear, and replace it if necessary.
Instruments with piston or spring mechanisms
- Clean instruments with piston or spring mechanisms after each use, using a mild detergent solution or an enzymatic cleaner.
- Lubricate the mechanisms periodically to reduce friction and maintain optimal performance.
- Inspect the instruments for any damage or wear, and replace them if necessary.
By following these regular maintenance tasks, healthcare professionals can ensure that surgical instruments remain in good condition and continue to provide safe and effective care to patients.
When to perform routine maintenance and service tasks
Surgical instruments are complex devices that require regular maintenance and servicing to ensure they function properly and safely. Routine maintenance tasks should be performed according to the manufacturer’s guidelines and should include:
- Inspecting instruments for damage or wear and tear
- Cleaning and disinfecting instruments after each use
- Lubricating moving parts
- Adjusting and tightening screws and other components
- Calibrating electronic instruments
Regular servicing tasks should also be performed, which may include:
- Replacing worn or damaged parts
- Sharpening blades and other cutting edges
- Re-calibrating electronic instruments
- Repairing any damage or defects
It is important to note that all maintenance and servicing tasks should be performed by trained professionals who are familiar with the specific requirements of each instrument. This ensures that the instruments are handled and maintained properly, and that any repairs are carried out safely and effectively.
Additionally, a schedule for routine maintenance and servicing should be established and followed to ensure that all instruments are properly maintained and ready for use when needed. This schedule should take into account the frequency of use, the complexity of the instruments, and the manufacturer’s guidelines.
The role of professional service and repair in instrument care
In addition to regular cleaning and maintenance, it is essential to consider professional service and repair for surgical instruments. Here are some key points to consider:
- Regular service and repair can help prevent breakdowns and extend the lifespan of instruments.
- Professional technicians have the knowledge and experience to properly diagnose and fix any issues with instruments.
- Repairs made by unauthorized individuals can void warranties and compromise the integrity of the instrument.
- Scheduled maintenance and repair appointments can ensure that instruments are always in optimal condition for use.
- Professional service and repair can also help to maintain compliance with regulations and standards for medical equipment.
Overall, the role of professional service and repair in instrument care cannot be overstated. By taking advantage of these services, healthcare facilities can ensure that their surgical instruments are always in the best possible condition for use.
Best Practices for Instrument Storage and Organization
Factors to consider when designing an instrument storage area
When designing an instrument storage area, several factors must be considered to ensure the proper care and preservation of surgical instruments. These factors include:
- Space Requirements: The available space for the storage area must be sufficient to accommodate all the instruments and equipment without any congestion or overcrowding. This allows for easy access and maneuverability, reducing the risk of damage or injury during handling.
- Temperature and Humidity Control: Surgical instruments are delicate and can be easily damaged by extreme temperatures or humidity levels. The storage area should be designed to maintain a consistent temperature and humidity level that is appropriate for the instruments being stored.
- Lighting: Adequate lighting is essential for proper inspection and cleaning of surgical instruments. The storage area should be well-lit to allow for easy identification of instruments and to detect any signs of damage or wear.
- Ventilation: Good ventilation is necessary to prevent the buildup of dust, moisture, and other contaminants that can damage instruments over time. The storage area should be designed to allow for proper air circulation, with sufficient filters to remove any airborne particles.
- Accessibility: The storage area should be easily accessible to authorized personnel for inspection, cleaning, and maintenance of the instruments. It should be located in a secure area to prevent unauthorized access or theft.
- Materials and Surfaces: The storage area should be constructed with materials that are non-corrosive, non-reactive, and easy to clean. Surfaces should be smooth and impervious to moisture, and any shelving or storage units should be designed to provide proper support and protection for the instruments.
- Storage Methods: The instruments should be stored in a manner that protects them from damage and prevents contamination. This may include using individual protective covers or containers, storing instruments in designated slots or bins, or using specialized storage systems designed specifically for surgical instruments.
By considering these factors when designing an instrument storage area, healthcare facilities can ensure the proper care and preservation of their surgical instruments, ultimately improving patient safety and reducing the risk of surgical complications.
Proper labeling and documentation of instruments
Effective labeling and documentation of surgical instruments are crucial for maintaining their proper identification and ensuring that they are readily available for use when needed. Here are some best practices for proper labeling and documentation of surgical instruments:
- Use clear and legible labels: The labels used to identify surgical instruments should be clear and legible to prevent confusion and ensure that they can be easily read by healthcare professionals.
- Include instrument identification numbers: Each surgical instrument should be assigned a unique identification number to facilitate proper tracking and organization.
- Use color-coding: Color-coding instruments can help healthcare professionals quickly identify instruments and differentiate them from one another. For example, all scalpels can be color-coded with a blue label, while all scissors can be color-coded with a red label.
- Maintain accurate documentation: Surgical instrument documentation should be accurate and up-to-date to ensure that instruments are properly tracked and available for use when needed. This documentation should include information such as the instrument’s identification number, manufacturer, model number, and maintenance history.
- Keep records organized and easily accessible: Records of surgical instrument maintenance and repair should be organized and easily accessible to ensure that they can be quickly referenced when needed. This information should be stored in a central location and should be easily searchable by instrument identification number or name.
By following these best practices for proper labeling and documentation of surgical instruments, healthcare professionals can ensure that instruments are easily identifiable, properly tracked, and readily available for use when needed. This can help to improve patient care and safety, while also maximizing the efficiency and effectiveness of surgical procedures.
Implementing a system for instrument tracking and rotation
To ensure the longevity and efficiency of surgical instruments, it is essential to implement a system for instrument tracking and rotation. This involves monitoring the usage and storage of instruments to prevent damage and maintain their optimal performance.
One effective method for instrument tracking and rotation is to create a checklist or inventory of all instruments and their respective uses. This checklist should be updated regularly to reflect any changes in the inventory or new instruments that have been added.
Another best practice is to assign specific instruments to specific procedures. This helps to reduce the risk of cross-contamination and ensures that the correct instruments are available when needed. Additionally, it is important to store instruments in a way that allows for easy access and visibility, such as in labeled containers or on a rack system.
To further optimize instrument tracking and rotation, some facilities utilize software programs that allow for real-time monitoring of instrument usage and availability. These programs can also generate reports to help identify any issues or inefficiencies in the instrument management process.
By implementing a system for instrument tracking and rotation, healthcare facilities can improve the overall quality and safety of patient care while also maximizing the lifespan of their surgical instruments.
Ensuring Compliance with Industry Standards and Regulations
Key regulatory requirements for surgical instrument care
In the healthcare industry, there are numerous regulatory requirements that govern the care and maintenance of surgical instruments. Compliance with these requirements is crucial to ensure patient safety and prevent the spread of infection. Here are some of the key regulatory requirements for surgical instrument care:
The Centers for Disease Control and Prevention (CDC) Guidelines
The CDC guidelines provide recommendations for the safe handling and processing of surgical instruments. These guidelines include strict protocols for cleaning and sterilization, as well as recommendations for the use of personal protective equipment (PPE) by healthcare personnel.
The Joint Commission
The Joint Commission is a national accreditation organization that sets standards for healthcare organizations in the United States. They require healthcare facilities to have policies and procedures in place for the cleaning and maintenance of surgical instruments, as well as guidelines for the use of PPE.
The Food and Drug Administration (FDA)
The FDA regulates the manufacture and sale of medical devices, including surgical instruments. They require manufacturers to meet certain performance standards and provide clear labeling and instructions for use.
Occupational Safety and Health Administration (OSHA)
OSHA sets standards for workplace safety, including the use of PPE and the handling of hazardous materials. Healthcare facilities must comply with OSHA regulations to ensure the safety of their employees and prevent the spread of infection.
In addition to these regulatory requirements, healthcare facilities must also adhere to industry standards and best practices for surgical instrument care. This includes following manufacturer guidelines for cleaning and maintenance, as well as implementing infection control procedures such as sterilization and disinfection. By ensuring compliance with these requirements, healthcare facilities can help prevent the spread of infection and ensure patient safety.
The role of training and education in maintaining compliance
Effective training and education programs play a crucial role in ensuring compliance with industry standards and regulations related to surgical instrument care. By providing staff members with the knowledge and skills necessary to properly clean, maintain, and store surgical instruments, healthcare facilities can reduce the risk of infection and maintain the highest levels of patient safety.
One key aspect of training and education is to ensure that all staff members understand the importance of proper instrument care and the potential consequences of failing to follow established protocols. This includes educating staff members on the specific requirements of industry standards and regulations, such as the Centers for Disease Control and Prevention (CDC) guidelines for reprocessing reusable medical devices.
In addition to educating staff members on industry standards and regulations, training and education programs should also focus on practical skills and techniques for cleaning, maintaining, and storing surgical instruments. This may include demonstrations of proper cleaning techniques, hands-on practice with instrument care equipment, and interactive simulations to reinforce key concepts.
By providing comprehensive training and education programs, healthcare facilities can ensure that all staff members are well-equipped to maintain the highest standards of surgical instrument care. This not only helps to protect patient safety, but also ensures that healthcare facilities are in compliance with industry standards and regulations.
The benefits of implementing a quality management system for instrument care
Implementing a quality management system (QMS) for surgical instrument care can provide numerous benefits, including:
- Compliance with industry standards and regulations: A QMS ensures that the organization follows industry standards and regulations related to surgical instrument care. This can help to avoid costly fines and legal issues, and can improve the organization’s reputation.
- Reduced risk of patient harm: By implementing a QMS, the organization can reduce the risk of patient harm due to contaminated or improperly maintained surgical instruments. This can lead to improved patient outcomes and satisfaction.
- Improved efficiency and productivity: A QMS can help to streamline processes related to surgical instrument care, reducing the time and resources required to maintain instruments. This can lead to improved efficiency and productivity within the organization.
- Increased employee satisfaction and retention: Employees who are involved in the development and implementation of a QMS may feel more engaged and satisfied with their work. This can lead to increased employee retention and reduced turnover.
- Enhanced reputation and credibility: By implementing a QMS, the organization can demonstrate its commitment to providing high-quality care and can enhance its reputation and credibility within the healthcare community.
Tips for Improving Your Surgical Instrument Care Process
Identifying areas for improvement in your current process
Effective surgical instrument care requires continuous evaluation and improvement of current processes. Identifying areas for improvement can help optimize your workflow and reduce the risk of instrument damage or contamination. Here are some tips for assessing your current process:
- Document your current process: The first step in identifying areas for improvement is to document your current process. This includes mapping out the steps involved in cleaning, maintaining, and storing surgical instruments, as well as identifying the personnel responsible for each step.
- Assess your current process: Once you have documented your current process, it’s important to assess its effectiveness. This can involve evaluating the time and resources required for each step, as well as identifying any bottlenecks or areas where instruments may be at risk of damage or contamination.
- Evaluate your team’s performance: Your team’s performance is a critical factor in the success of your surgical instrument care process. Evaluate their performance by monitoring their adherence to your documented process, as well as their ability to identify and address issues that arise.
- Consider the needs of your organization: Your surgical instrument care process should be tailored to the needs of your organization. Consider factors such as the volume of procedures performed, the types of instruments used, and the unique needs of your surgical team when evaluating your current process.
- Seek feedback from your team: Your team’s input is valuable when it comes to identifying areas for improvement in your surgical instrument care process. Seek feedback from them on a regular basis, and use their input to make changes and improvements to your process.
By following these tips, you can identify areas for improvement in your current surgical instrument care process and make changes that will help optimize your workflow and reduce the risk of instrument damage or contamination.
Implementing new technologies and tools to enhance instrument care
- Advancements in technology have revolutionized the field of surgical instrument care, offering healthcare professionals a range of new tools and techniques to improve the efficiency and effectiveness of their processes.
- Some examples of new technologies and tools that can be used to enhance instrument care include automated cleaning and sterilization systems, digital inventory management software, and advanced lubricants and coatings that can extend the life of instruments and reduce friction.
- Investing in these new technologies and tools can help to streamline the instrument care process, reduce the risk of errors and complications, and ensure that instruments are always in top condition for use in surgical procedures.
- However, it is important to note that these technologies and tools should be used in conjunction with established best practices for cleaning, maintenance, and storage to ensure the best possible outcomes.
- Additionally, it is important to stay up-to-date with the latest developments in surgical instrument care technology and to continuously evaluate and assess the effectiveness of these technologies and tools in order to optimize the instrument care process and improve patient outcomes.
The role of staff training and education in continuous improvement
Effective surgical instrument care is a critical aspect of patient safety and operational efficiency in any healthcare facility. While having the right tools and equipment is essential, it is equally important to ensure that your staff is adequately trained and educated on the best practices for cleaning, maintenance, and storage of surgical instruments. In this section, we will discuss the role of staff training and education in continuous improvement of surgical instrument care.
Training and education play a crucial role in ensuring that healthcare providers understand the importance of proper instrument care and the procedures involved in maintaining them. Continuous improvement of surgical instrument care involves providing ongoing training and education to staff to ensure that they are up-to-date with the latest best practices and standards. This includes providing training on the proper use and handling of instruments, as well as educating staff on the latest technologies and techniques for cleaning and sterilizing instruments.
Continuous improvement of surgical instrument care also involves creating a culture of accountability and responsibility among staff. This means that everyone involved in the care and handling of surgical instruments must be aware of their role in maintaining their quality and safety. This includes providing feedback and recognition for staff who demonstrate excellence in instrument care, as well as addressing any issues or concerns that may arise.
Creating a culture of continuous improvement also involves regular evaluation and assessment of instrument care processes. This includes reviewing and updating policies and procedures, as well as conducting regular audits to ensure that best practices are being followed. By involving staff in these evaluations and assessments, you can create a sense of ownership and accountability for the quality of instrument care in your facility.
In addition to these strategies, it is also important to provide ongoing support and resources for staff to ensure that they have the tools and information they need to provide the best possible care for surgical instruments. This may include providing access to training materials, instructional videos, and other resources that can help staff stay up-to-date with the latest best practices and standards.
Overall, the role of staff training and education in continuous improvement of surgical instrument care cannot be overstated. By providing ongoing training and education, creating a culture of accountability and responsibility, and regularly evaluating and assessing instrument care processes, you can ensure that your staff is equipped to provide the best possible care for surgical instruments and ultimately, improve patient safety and operational efficiency in your healthcare facility.
Summarizing the key points of the guide
To ensure the best possible surgical outcomes, it is crucial to prioritize the care and maintenance of surgical instruments. Here are the key takeaways from this guide:
- Regular cleaning and sterilization: Surgical instruments should be cleaned and sterilized regularly to prevent the buildup of bacteria and other contaminants. This should be done in accordance with the manufacturer’s instructions and guidelines.
- Proper storage: Surgical instruments should be stored in a clean, dry, and well-ventilated area. They should be arranged in a way that allows for easy access and prevents damage to the instruments.
- Inspection and maintenance: Regular inspection and maintenance of surgical instruments can help identify any issues before they become major problems. This includes checking for signs of wear and tear, as well as ensuring that all components are functioning properly.
- Education and training: All members of the surgical team should be educated and trained on the proper care and maintenance of surgical instruments. This includes understanding the importance of regular cleaning and sterilization, as well as the proper techniques for handling and storing instruments.
- Adherence to guidelines and regulations: Surgical instrument care should always adhere to relevant guidelines and regulations, such as those set forth by the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
By following these best practices, healthcare facilities can ensure that their surgical instruments are always in good working order, which can lead to better patient outcomes and a safer surgical environment.
The ongoing importance of proper surgical instrument care for patient safety and healthcare provider success
- Ensuring the sterility of surgical instruments is crucial for preventing infections and maintaining patient safety.
- The improper handling or cleaning of surgical instruments can lead to cross-contamination, which can pose a significant risk to patients and healthcare providers.
- Regular maintenance and storage of surgical instruments can help extend their lifespan and ensure they are always ready for use when needed.
- Investing in quality surgical instrument care processes can also help healthcare providers save time and money in the long run by reducing the need for costly repairs or replacements.
- Ultimately, proper surgical instrument care is essential for ensuring the success of healthcare providers and the well-being of their patients.
FAQs
1. What are the best practices for cleaning surgical instruments?
Cleaning surgical instruments is crucial to prevent the spread of infection and maintain instrument quality. The best practices for cleaning surgical instruments include:
* Using a validated cleaning process that removes all soil, blood, and other biological matter.
* Using a detergent that is compatible with the instrument material and does not damage the instrument’s finish.
* Rinsing the instrument thoroughly with water to remove all soap residue.
* Drying the instrument with a clean, dry cloth or paper towel to prevent corrosion.
* Inspecting the instrument for any remaining debris or residue before moving on to the next step in the reprocessing cycle.
2. How often should surgical instruments be maintained?
Surgical instruments should be maintained regularly to ensure they are in good working condition and to prevent damage. Maintenance should be performed at least once a year, or more frequently if the instruments are used frequently or in high-risk procedures.
3. What is the best way to store surgical instruments?
Surgical instruments should be stored in a clean, dry place with good ventilation to prevent corrosion. Instruments should be stored in a way that allows for easy access and prevents damage to the instruments. It is also important to store instruments in a way that prevents the spread of infection, such as using sterile storage containers for sterilized instruments.
4. How can I prevent damage to surgical instruments during cleaning and maintenance?
To prevent damage to surgical instruments during cleaning and maintenance, it is important to follow the manufacturer’s instructions for use and reprocessing guidelines. This includes using the correct cleaning agents and tools, and avoiding exposing the instruments to excessive heat, moisture, or chemicals. It is also important to inspect the instruments regularly for any signs of damage and report any issues to the instrument maintenance team.
5. What should I do if I notice signs of damage on a surgical instrument?
If you notice any signs of damage on a surgical instrument, such as rust, corrosion, or bent parts, you should report it to the instrument maintenance team immediately. Damaged instruments should not be used in patient care and should be repaired or replaced as soon as possible to prevent the spread of infection and ensure the safety of patients.